vintage Bernings Sho lace up fur coat
(税込) 送料込み
商品の説明
◯ブランド
Bernings Sho
◯商品名
Bernings Sho バーニング ショー
ファー レースアップ デザイン コート
◯サイズ
着丈約85cm 身幅約57.5cm 肩幅約43.5cm
袖丈約61.5cm
◯色
画像参照
※タグ付き、未使用品
★フォロー割
フォローして下さった方には、商品価格に応じてお値引きさせて頂きます。
【ご購入前】にコメント欄にフォローしたことをお知らせ下さい。
⚫︎3,以下→OFF
⚫︎3,以上→OFF
⚫︎10,以上→OFF
すでにフォロー頂いている方には毎回適応致しますので都度コメント欄よりお伝え下さい!
★まとめ割引
まとめ買いでさらにお値引き、させて頂きますので、コメント欄にご相談下さい!
ほぼ全ての商品はusedになります。
used品に理解のある方のみ購入お願いします。
全購入者様は商品説明、プロフィールを読んだとみなし販売しております。
mxxshopでは 70s 70年代 80s 80年代 90s 90年代 00s 2000年代 の vintage
ヴィンテージ ビンテージ 古着 モード ストリート アメカジ と様々なジャンルの洋服、アクセサリーの販売をしています。
【取り扱いブランド】
ナイキ アディダス チャンピオン ジョーダン ラルフローレン トミー ヒルフィガー ユニクロ ノーティカ ポールスミス ノースフェイス パタゴニア カーハート ステューシー スラッシャー
【取り扱いアイテム】
ナイロンジャケット パーカー ジャージ トラックジャケット フーディ スウェット トレーナー ジャケット デニム デニムシャツ デニムジャケット ネルシャツ シャツ ブルゾン スイングトップ コーチジャケット マウンテンパーカー ワークシャツ スタジャン y2k ベルト
古着 used ビックシルエット オーバーサイズ ドロップショルダー ワイドスリーブ 銀タグ ビックロゴ デカロゴ メンズ レディース ビンテージ ゆるだぼ ワンピース チュニック ロング丈 ワンピ USサイズ ヴィンテージ 大きいサイズ 古着男子 古着女子
興味がありましたら下記ハッシュタグにまとめています。
↓こちらで私の全出品を確認できます。
#mxxshop商品の情報
| カテゴリー | メンズ > ジャケット/アウター > トレンチコート |
|---|---|
| 商品のサイズ | M |
| ブランド | ヴィンテージ |
| 商品の状態 | 未使用に近い |

mxxshopvintage Bernings Sho lace up fur coat - トレンチコート

Vintage Eastern Furriers Fur Coat, Made in Canada

Strait Jacket BDSM Pure Leather Jacket for Men/women Strait Jacket

Vintage Black Sheared Beaver Fur Coat B169 With Mink Collar

Japanese brand berning sho - Gem
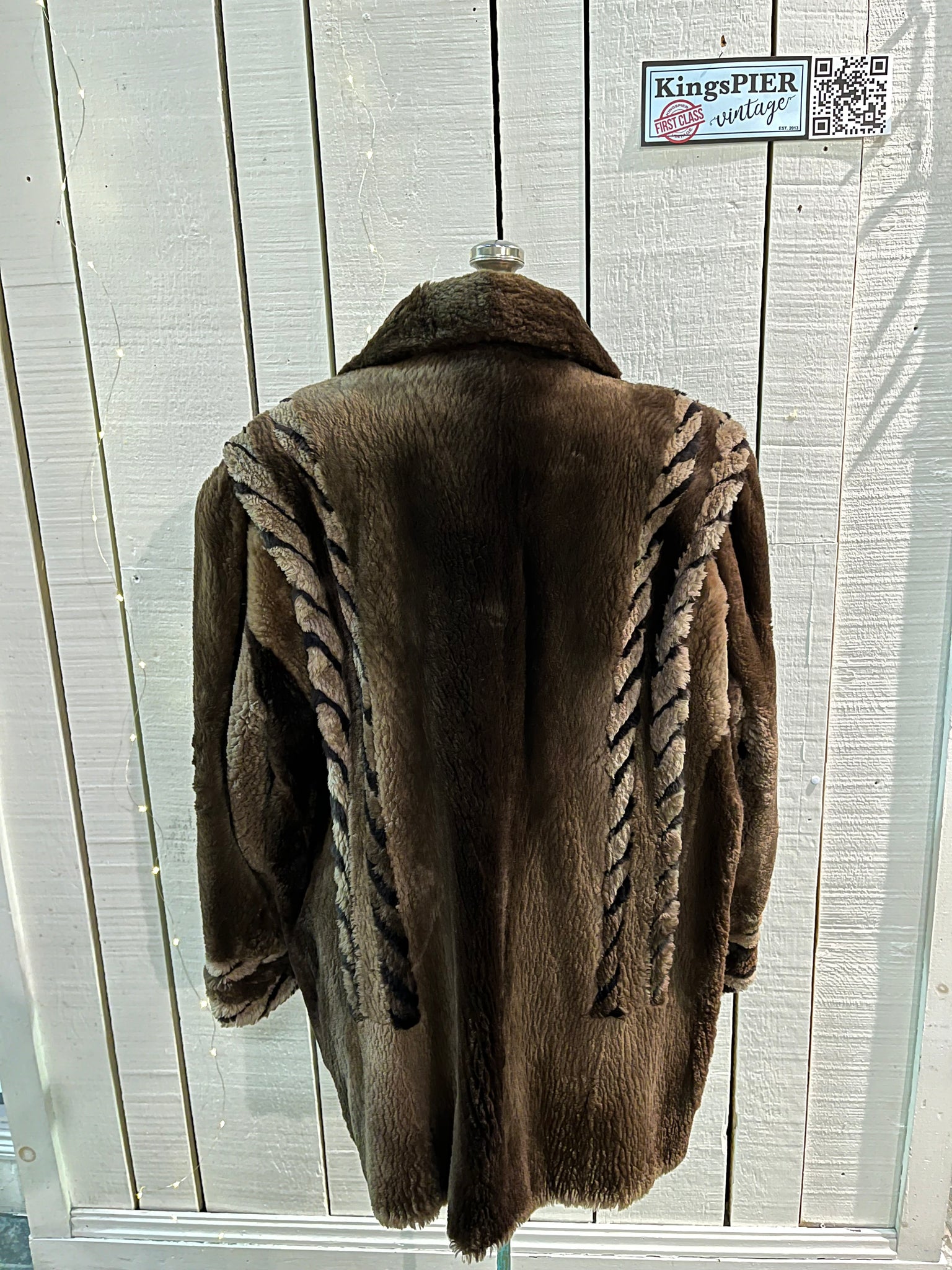
Vintage Eastern Furriers Fur Coat, Made in Canada – KingsPIER vintage

2024年最新】bernings sho バーニングショーの人気アイテム - メルカリ

Japanese brand berning sho - Gem

Bernings Sho - Etsy Canada

Stunning vintage 1940's or 50's shorn beaver fur coat. Made in Saint John, New Brunswick, Canada

Shoes, $1330 at us.louisvuitton.com - Wheretoget | Fur street

Berning Sho | Grailed

Japanese brand berning sho - Gem

Brand New Luxurious Pastel Swing Canadian Mink Fur Coat Stroller M

Vintage Penny Lane Coat | Fur Cuff | Fur Collar | Suede | Brown

Berning Sho | Grailed

Vintage Leonard Cobalt Mongolian Fur Short Sleeve Swing Coat – Recess

Vintage 1960s SHEARLING SHERPA Suede lace Up Boots // Hush Puppies

Best 25+ Deals for Vintage Fur Coats For Sale | Poshmark

Vintage Eastern Furriers Fur Coat, Made in Canada – KingsPIER vintage

Vintage Coats & Jackets For Sale | Women's, Leather & Retro – Shop

Pre Owned Mink Coats– Purple Shoshana Furs

100+ affordable

Vintage Black Sheared Beaver Fur Coat B169 With Mink Collar - Etsy
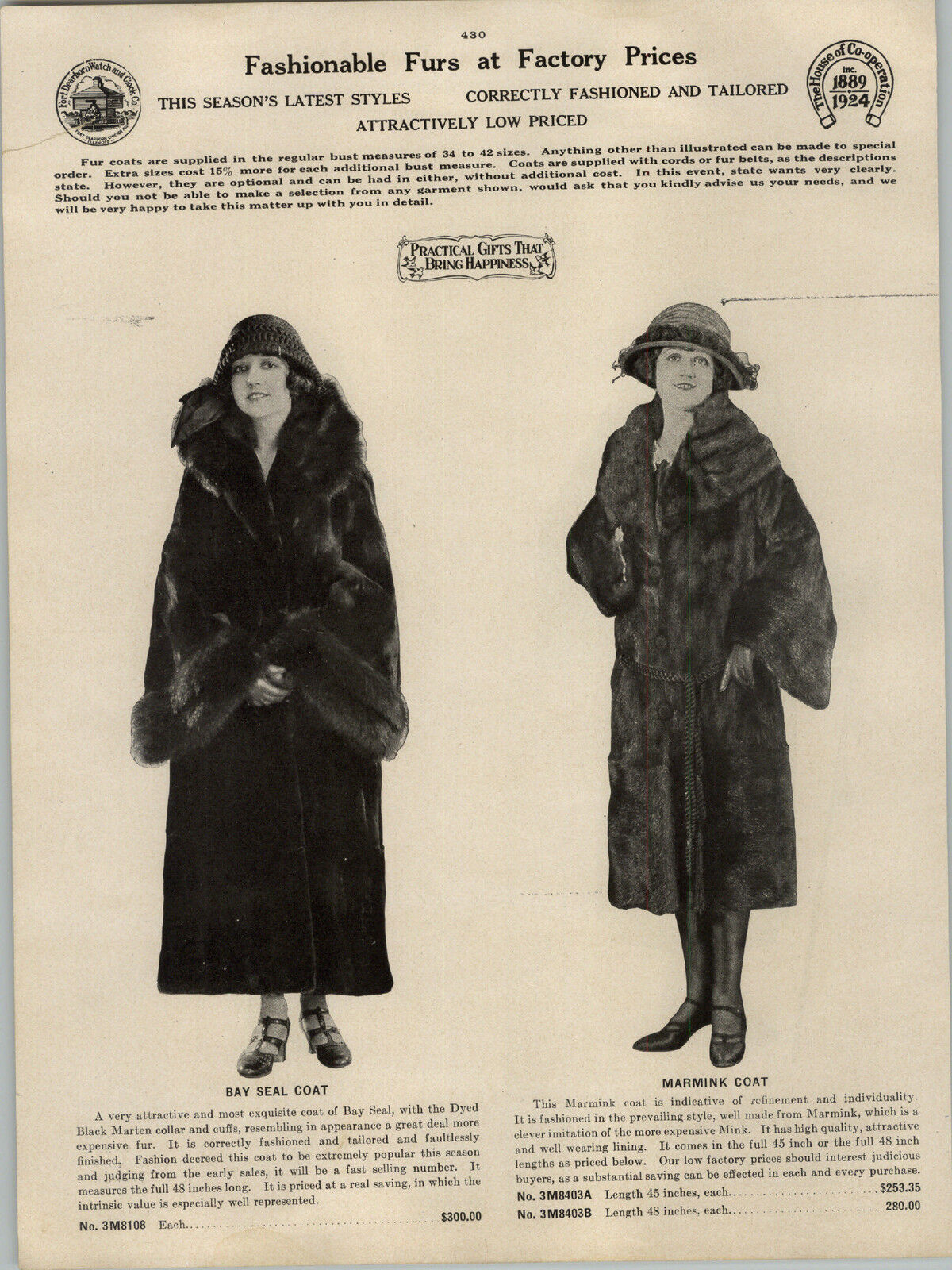
1924 PAPER AD 11 PG Stylish Fur Coat Coats Mink Bay Hudson

Best 25+ Deals for Vintage Fur Coats For Sale | Poshmark

Vintage rare🔥bernings sho design - Gem

Vintage Coats & Jackets For Sale | Women's, Leather & Retro – Shop

Berning Sho | Grailed

vintage Persian lamb fur coat – 86 Vintage

Vintage Original Black Ribbon Knit Short Jacket With White Mink

Couture Hélène Vintage 80s Belgium Made Spectacular Vegan Fur

Vintage AUTUNNO I. J. Fox Boston Rex Rabbit Fur, Leather & Fabric

Brand New Luxurious Pastel Swing Canadian Mink Fur Coat Stroller M

vintage fur coats in All Categories in Alberta - Kijiji Canada

Vintage Simpsons Brown Mink Three Quarter Cut Jacket, Mink Fur

Le Thrift Consignment : Fashion Focus: Vintage Fur

Jet Set Sewing | Jet Set Sewing | Page 2

Best 25+ Deals for Vintage Fur Coats For Sale | Poshmark

Vintage


















商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














