Louis Vuitton
(税込) 送料込み
商品の説明
商品の説明はありません
商品の情報
| カテゴリー | レディース > トップス > シャツ/ブラウス(半袖/袖なし) |
|---|---|
| 商品のサイズ | S |
| ブランド | ルイヴィトン |
| 商品の色を | グレイ系 / ブラック系 |
| 商品の状態 | 新品、未使用 |

Neverfull GM Monogram - Women - Handbags | LOUIS VUITTON ®

Onthego GM Monogram Giant Canvas, Brownn | LOUIS VUITTON ®

OnTheGo PM Monogram Canvas - Women - Handbags | LOUIS VUITTON ®

Multi Pochette Accessoires Monogram - Women - Handbags | LOUIS

Pochette Métis Monogram - Women - Handbags | LOUIS VUITTON ®
Louis Vuitton, exceptional ready-to-wear - Fashion & Leather Goods

OnTheGo GM Bicolor Monogram Empreinte Leather - Women - Handbags

OnTheGo MM Bicolor Monogram Empreinte Leather - Women - Handbags

CarryAll PM Monogram - Women - Handbags | LOUIS VUITTON ®

Pochette Accessoires Monogram - Women - Small Leather Goods

Neverfull MM Damier Ebene - Women - Handbags | LOUIS VUITTON ®

Graceful MM Women's Hobo Handbags | LOUIS VUITTON ®

OnTheGo MM Monogram - Women - Handbags | LOUIS VUITTON ®

Petit Palais Monogram - Women - Handbags | LOUIS VUITTON ®

Boulogne Monogram - Women - Handbags | LOUIS VUITTON ®

Alma PM Monogram - Women - Handbags | LOUIS VUITTON ®

Speedy Bandoulière 20 Monogram - Women - Handbags | LOUIS VUITTON ®

Camera Box Other Monogram Canvas - Women - Handbags | LOUIS VUITTON ®

Favorite Bicolor Monogram Empreinte Leather - Women - Handbags

Loop Hobo Monogram Canvas - Women - Handbags | LOUIS VUITTON ®

LeBron James Wore a $28,000 Louis Vuitton Fit to Celebrate His New

Palm Springs Mini Monogram - Women - Handbags | LOUIS VUITTON ®

Vanity PM Other Monogram Canvas - Women - Handbags | LOUIS VUITTON ®

OnTheGo East West Monogram Reverse - Women - Handbags | LOUIS

Louis Vuitton (designer) - Wikipedia

Vénus Monogram - Women - Handbags | LOUIS VUITTON ®

NéoNoé MM Bicolor Monogram Empreinte Leather - Women - Handbags
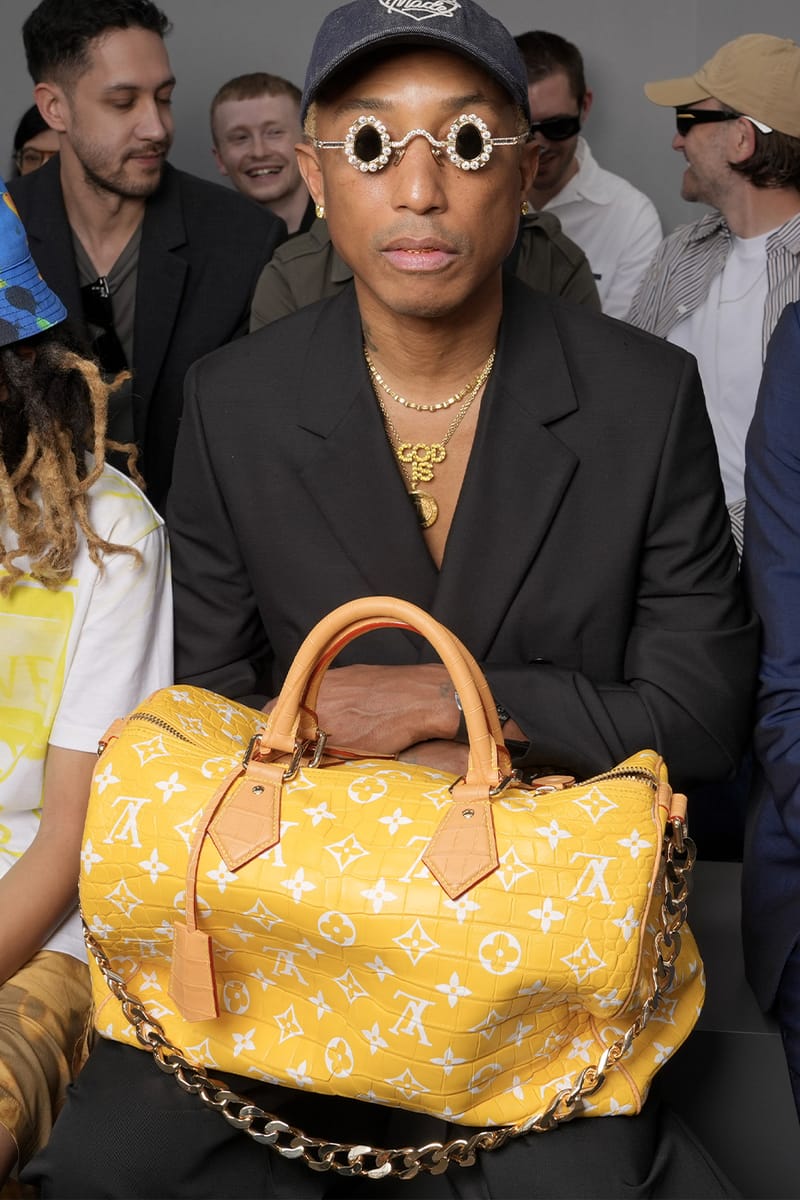
Pharrell $1 Million Louis Vuitton Speedy Bag 4 New Colors | Hypebeast

Louis Vuitton Fall 2024 Menswear Collection | Vogue

Speedy 30 Monogram - Women - Handbags | LOUIS VUITTON ®

Loop Monogram - Women - Handbags | LOUIS VUITTON ®

Luxury Monogram Canvas and Leather Handbag Neonoe | LOUIS VUITTON ®

Louis Vuitton's Speedy Is the Latest It Bag in Menswear, Here's

The Anatomy of the Louis Vuitton Bumbag - Academy by FASHIONPHILE

Cluny BB Monogram - Women - Handbags | LOUIS VUITTON ®

Neverfull MM Damier Ebene - Women - Handbags | LOUIS VUITTON ®

Nice Vanity Monogram Canvas - Women - Travel | LOUIS VUITTON ®

Keepall Bandoulière 55 Monogram Canvas - Women - Travel | LOUIS

Petite Malle Souple Monogram - Women - Handbags | LOUIS VUITTON ®

Luxury Totes for Women - Women's Designer Tote Bags - LOUIS VUITTON ®



商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














