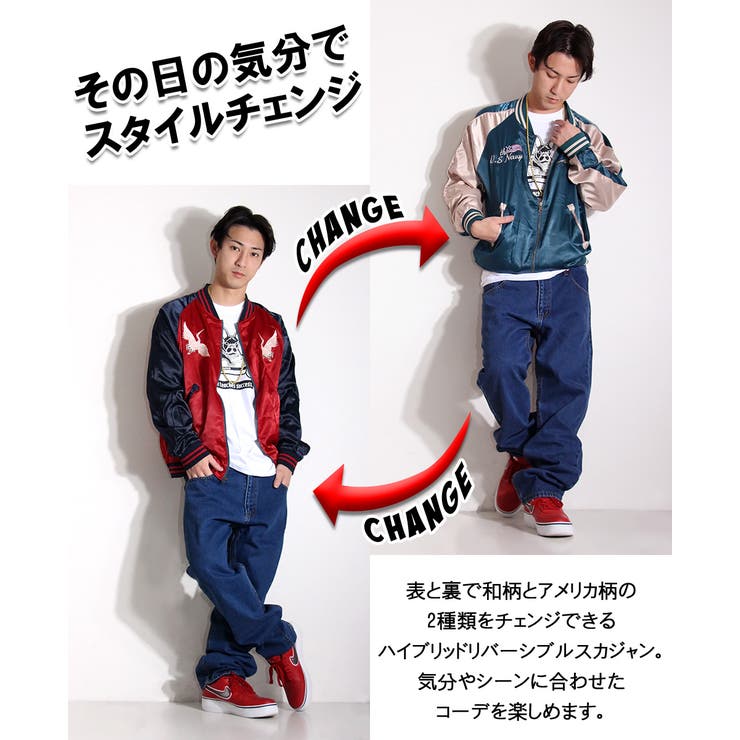
スカジャン リバーシブル
(税込) 送料込み
商品の説明
フード···フードなし
カラー···ブルー
季節感···冬
モンストスカジャン蓬莱リバーシブル商品の情報
| カテゴリー | メンズ > ジャケット/アウター > スカジャン |
|---|---|
| 商品のサイズ | L |
| 商品の色を | ブルー系 / ホワイト系 |
| 商品の状態 | 未使用に近い |

カラーブルースカジャン リバーシブル - スカジャン

リバーシブルスカジャン
![楽天市場】刺繍スカジャン [リバーシブル] 《楽天イーグルス》 : 楽天](https://tshop.r10s.jp/rakuteneagles/cabinet/itemimg/2020_7/b0100048_a.jpg)
楽天市場】刺繍スカジャン [リバーシブル] 《楽天イーグルス》 : 楽天

スカジャン【DIESEL】 リバーシブル スカジャン - スカジャン

スカジャン リバーシブル - アウター

試着対象】リバーシブルスーベニアジャケット / スカジャン|ALPHA|アルファ

楽天市場】男女兼用 仙鶴刺繍マーク スカジャン リバーシブル 横須賀

楽天市場】<送料無料>【LiN】“お友達” 総刺繍 リバーシブル

スカジャン リバーシブル かっこいい ユニセックス ロゴ S~3XL

スカジャン リバーシブル 別珍 寅キルティング メンズ スカジャン 純正

アヴィレックス スカジャン(リバーシブル)メンズ - スカジャン

Amazon | スタジャン ジャケット コート スカジャン 1 M リバーシブル

リバーシブル刺繍スカジャン(ブルゾン/ジャンバー) | tk.TAKEO

スカジャン リバーシブル-

高須クリニック(Lサイズ)スカジャン(リバーシブルタイプ)【8月下旬発送
スカジャン リバーシブル 鶴

LDY in Wonder Land 刺繍リバーシブルスカジャン|ランドリーTシャツ

最旬ダウン スカジャン リバーシブル 初期M品番 テーラー東洋 テーラー
爆売中 スカジャン メンズ 40代 スカジャン リバーシブル ジャンバー ライオンキング柄 刺繍 和柄 横須賀風 ポリエステル 長袖 サテン アウター 軽量 : so419673229d4 : R商事 - 通販 - Yahoo!ショッピング

今昔 こんじゃく 和柄 スカジャン リバーシブル メンズ きつね 梅 刺繍

スプラトゥーン2/リバーシブルスカジャン - EDITMODE ONLINE STORE
スカジャン リバーシブル - アウター

RINGS】 リバーシブルスカジャン (133154) | rings-official

スカジャン リバーシブル 虎 ヴィンテージ - アウター

ヴィンテージ スカジャン リバーシブルスーベニア別珍 - スカジャン

LAUNDRY百鬼夜行 リバーシブルスカジャン|ランドリーTシャツ公式通販

スカジャン(リバーシブル)スカジャン - bluechipbr.com

特価情報 スカジャン リバーシブル -スカジャン

高須クリニック(XXLサイズ)スカジャン(リバーシブルタイプ)【8月下旬

泥棒日記 スカジャン リバーシブル-

未使用品 抜刀娘 スカジャン リバーシブル ネイビーピンク 裏ブラック

AIVER リバーシブル鬼スカジャン(スカジャン)|AIVER(アイバー)の

新しいコレクション スカジャン リバーシブル | concessionariareviver

スカジャン リバーシブルスカジャン - www.kairosinsurancegroup.com

3RSJ-501 地図青龍リバーシブルスカジャン - スカジャンのショッピング

スカジャン リバーシブル 絡繰魂の通販・価格比較 - 価格.com

スカジャンEVISUスカジャンリバーシブル42 - ブルゾン

花旅楽団 ハナタビガクダン 和柄 スカジャン リバーシブル メンズ 総刺繍

東洋エンタープライズ - 東洋エンタープライズ スカジャン

PACMAN 日本地図スカジャン(リバーシブル)|OTHERS(アザーズ




商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています














